|
By Ben Paul The Patient Protection and Affordable Care Act, commonly called Obamacare, continues to be the most controversial policy intervention in recent history. The public remains evenly split on the law, and its detractors continue to obstruct its implementation at every turn. Yet, we’ve overlooked one central achievement of the law. Obamacare has led to a dramatic reduction in preventable adverse events (PAEs). This revolution has saved tens of thousands of lives and billions in unnecessary health care costs. A preventable adverse event is any medical condition or complication acquired in a hospital that better care could have prevented. Examples of PAEs include infections acquired while at the hospital, patient falls, and incorrect drug dosages. One misnomer people have about PAEs is that they are usually a consequence of neglect. In reality, they are typically due to poorly designed care systems that set up health care providers for failure. For example, there might not be standardized medical devices across or within hospitals, physician and nursing teams may be working together for the first time, or medical records may be poorly written and organized. 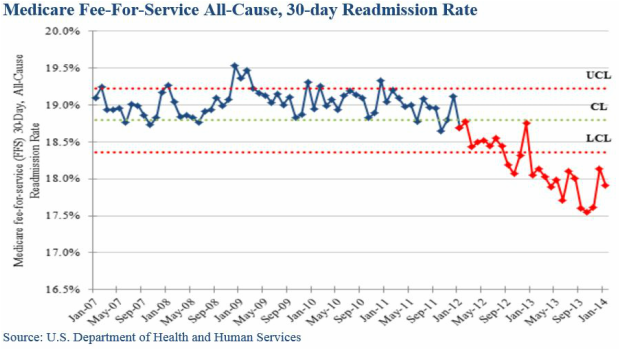 Preventable adverse events have plagued the United States. One study estimates between 210,000 and 400,000 hospital patients die each year due to PAEs, placing it in the top five leading causes of death in the United States. For context, heart disease is the leading annual cause of death for Americans, claiming approximately 600,000 lives each year. Another study found preventable adverse medical events occur in one-third of all hospital admissions. Preventable adverse events are costly, as patients who suffer for PAEs need additional care. Medical errors cost the United States economy an unnecessary $19.5 billion in 2008. These costs included additional medical spending to care for the adverse event as well as the lost economic value due to increased mortality rates and lost productivity. The total economic loss inflates to between $73.5 billion and $98 billion per year when applying quality-adjusted life years, a commonly used measurement to value disease burden, to PAEs. Obamacare’s architects recognized this problem and took unprecedented steps to solve it. The law authorized the government and stakeholders to develop quality measures to measure performance. It also directed Medicare to begin reimbursing providers based on the quality, not quantity, of care provided. Furthermore, the law prohibited the federal and state governments from paying doctors for treating infections developed in the hospital. Lastly, Obamacare introduced the hospital readmissions reduction program, which financially penalizes hospitals that have a disproportionate number of preventable readmissions. These measures have had their intended effect. The Department of Health and Human Services estimates there were 1.3 million fewer PAEs between 2010 and 2013, a 17 percent reduction, compared to the 2010 baseline. There was also an 8 percent reduction in preventable hospital readmissions among Medicare patients, as well as decreases in adverse drug reactions, patient falls, and central line infections. All told, the reduction in PAEs has saved as many as 50,000 lives and $12 billion. There is still work to do. Preventable adverse events are just that – preventable. Other industries including aviation and manufacturing have made great strides over the past several decades to significantly reduce the incidence of errors and harm. PAEs will continue to be a significant policy problem until they are as rare in these other fields.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Categories
All
Archives
April 2022
|
ADDRESSVirginia Policy Review
235 McCormick Rd. Charlottesville, VA 22904 |
|
SOCIAL MEDIA |